Abstract
Background: Sickle cell disease (SCD) is characterized by hemolytic anemia and a hyperdynamic circulation resulting in impaired cerebral hemodynamics and perfusion, culminating in ischemic damage of the brain. SCD is strongly associated with overt strokes or silent cerebral infarctions (SCI) which have been related to elevated flow in the median cerebral artery in children measured by transcranial Doppler. Patients with SCD have an increased cerebral blood flow (CBF) to maintain adequate oxygen delivery (OD). Previously, we and others have demonstrated with special MRI techniques that despite the maintained OD, cerebral metabolic rate of oxygen (CMRO2) is reduced in SCD due to reduced oxygen extraction fraction (OEF), which in turn is strongly related to CBF and hemoglobin (Hb) level. Voxelotor is a small molecule that reversibly binds to Hb and increases its oxygen affinity, thereby decreasing Hb polymerization and sickling. The resulting decreased hemolytic anemia can potentially ameliorate cerebral hemodynamics and perfusion, the increased oxygen affinity may reduce the offloading of oxygen.
The aim of our study is to assess the effects of voxelotor on markers of cerebral perfusion and oxygen metabolism. In addition, the effect of voxelotor on the hyperdynamic cardiac function was assessed.
Methods: This single-arm, interventional trial is being conducted in a tertiary hospital in Amsterdam, The Netherlands. Adult SCD patients with the severe genotypes of HbSS and HbSβ0-thalassemia were eligible for inclusion. Other major inclusion criteria were: Hb ≤ 10.5 g/dL and in case of hydroxyurea use, a stable dose for at least 90 days. Major exclusion criteria were: regular transfusions or a transfusion within 90 days prior to inclusion, hospitalization for vaso-occlusive crisis ≤ 14 days before inclusion. At baseline and after 3 months of voxelotor treatment (1500 mg pd), MRI scans, echocardiography and laboratory assessments were performed. Time-encoded arterial spin labeling was performed to obtain CBF measurements, gray matter CBF was derived by using white matter and gray matter masks. T2 relaxation under spin tagging was performed in order to calculate OEF. Oxygen delivery and CMRO2 were calculated: formula, CBF x OD, with the OD calculated from OEF and oxygen content. Maximal tricuspid regurgitation velocity (TRVmax) was assessed by trans-thoracic echocardiography as a marker of hyperdynamic circulation. N-Terminal pro-B-type natriuretic peptide (NT-proBNP) was measured as a marker of cardiac stress/dilatation. Parametric data are presented with mean and SD and analyzed by a paired T-test and non-parametric data with median and IQR, and analyzed by a Wilcoxon signed-rank test.
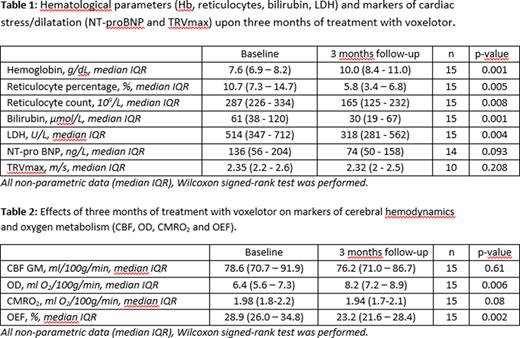
Results: Preliminary results of 15 patients (HbSS/HbSβ0-thalassemia, 11/4, mean age 38 years (SD 10), 4 female) who completed their 3 month follow-up are presented here. Upon 3 months of voxelotor treatment, Hb levels significantly increased, 7.6 g/dL, (IQR 6.9 - 8.2) compared to 10.0 g/dL (IQR; p < 0.001), and hemolysis significantly reduced, represented by reticulocyte count, bilirubin and LDH levels (p = < 0.05; Table 1). After 3 months of treatment also a significant increase in oxygen delivery from 6.4 to 8.2 ml O2/100g/min (p = 0.006) was observed, which was primarily due to the increased Hb levels. However, CBF and CMRO2 did not change significantly after 3 months of voxelotor treatment (Table 2) while OEF decreased significantly at 3 months as compared to baseline (from 28.9% to 23.2%, p = 0.002) (Table 2). No significant changes in NT-proBNP levels and TRVmax were observed (Table 1) although a significant decrease was observed in patients with NT-proBNP-levels >160 at baseline (213 (IQR 161 - 254) ng/L vs 152 (IQR 50 -163) ng/L; p = 0.028)).
Conclusion: In this preliminary study, no changes in cerebral hemodynamics (CBF) and oxygen metabolic rate (CMRO2) were observed, despite an increased cerebral oxygen delivery due to improvement of Hb levels. CMRO2 remained unchanged as a result of diminished OEF, based on the calibration according to the Li-Bush model, most likely due to the increased oxygen affinity attributed to voxelotor. With respect to the cardiac measures of the circulatory state, no effect on NT-proBNP levels and TRVmax was observed although a significant decrease in NT-proBNP-levels was observed in a post-hoc analysis of patients with elevated NTproBNP levels at baseline.
Disclosures
Nur:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Biemond:Celgene: Membership on an entity's Board of Directors or advisory committees; Chiesi: Membership on an entity's Board of Directors or advisory committees; BMS: Research Funding; CSL Behring: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Novo Nordisk: Membership on an entity's Board of Directors or advisory committees; Modus Therapeutics: Membership on an entity's Board of Directors or advisory committees; Chiesi: Membership on an entity's Board of Directors or advisory committees; CSL Behring: Membership on an entity's Board of Directors or advisory committees; Bluebird Bio: Membership on an entity's Board of Directors or advisory committees; GBT: Research Funding; Bluebird Bio: Membership on an entity's Board of Directors or advisory committees; Novo Nordisk: Membership on an entity's Board of Directors or advisory committees; BMS: Research Funding; GBT: Membership on an entity's Board of Directors or advisory committees, Research Funding; Sanquin: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.